This article is to discuss Osteoarthritis , ( synonym : Degenerative Arthritis Or osteoarthrosis Or degenerative joint disease ) regarding its definition, risk factors, pathology & pathogenesis, classification (types), Clinical picture (symptoms and signs), diagnostic investigations and treatment approach.
• Osteoarthritis (osteoarthrosis) may be primary or secondary. Usually it is the end result of a variety of pattern of joint failure.
• It is characterized by degeneration of articular cartilage with simultaneous proliferation of new bone, cartilage and connective tissue leading to remodelling of joint contour, inflammation of synovial membrane is minor and secondary.
 2- Aging.
2- Aging.
3- Genetic factors.
4- Obesity (loading stress on weight
bearing joint e.g. knee).
5- Smoking
2- Growth factors e.g insulin like growth factor and transforming growth factor are involved in stimulating collagen repair and production of the over growth at the joint margin (osteophytes).
• Cartilage is a matrix of collagen fibres enclosing a mixture of proteoglycans and.water .
• Under normal circumstances there is a dynamic balance between cartilage degradation by wear and its production by chondrocytes.
• Early, in cases of osteoarthritis the cartilage becomes fissured and ulcerated due to collagen matrix breakdown.
• Cartilage ulceration exposes underlying bone to increased stress producing rnicrofractures and cysts.
The bone attempts repair but produces abnormal sclerotic subchondral bone and over growth at joint margin called osteophytes.
• Localized.
• Generalized (3 or more joint areas)
2- Secondary osteoarthritis :-
• Mechanical e.g. occupational, hypermobility, cruciate tears.
• Metabolic: Haemochromatosis, Wilson's disease.
• Inflammatory: Rheumatoid arthritis, Gout, sero-ve arthropathy.
• Developmental: Epiphyseal dysplasia.
• Miscellaneous: Haemophilia, neuropathies.
Symptoms
Osteoarthritis affects many joints with insidious onset. Hip and knee osteoarthritis is the major cause of disability.
1- Pain (progressive i.e. months to years) which worsens with activity and is relived by rest.
2- Morning stiffness (brief < 15 minutes).
3- Gelling phenomenon refers to the sense of renewed stiffness in diseased joint after prolonged inactivity
Signs
1- Tenderness with limitation of range of movement (capsular thickening, blocking by osteophyte).
2- Crepitus on movement due to rough articular surfaces.
3- Joint enlargement due to soft tissue swelling or osteophytes.
4- Deformity e.g - Varus (medial angulation) , valgus (lateral angulation)
5- Joint effusion, wasting of muscles.
6- Osteoarthritis of the hands leading to:
• Heberden's nodes: Bony swelling of distal inter-phalyngeal joint.
• Bouchard's nodes: Bony swelling of proximal inter-phalyngeal joint.
• Rheumatoid factor and ANA are nagative
• X ray - Joint space narrowing (loss of cartilage).
- Marginal osteophytes.
- Subchondral sclerosis.
• MRI Showing early cartilage changes
• Arthroscopy can reveal surface erosion and fissuring of the cartilage.
• Weight loss, joint rest.
• Knee cage, cervical collar or lumbar corset.
• Exercise to support muscle around joint (the best is swimming), strengthening exercises for quadriceps.
• Heat modalities.
Pharmacologic therapy:
• Topical NSAIDs are safe and relatively effective.
• Oral paracetamol 1gm TDS and when needed, it is safe and welltolerated.
• Oral NSAIDs are more potent than paracetamol but they may lead to gastritis, peptic ulcer, nephrotoxicity.
• Oral glucosamine sulphate, may have chondroprotective effect.
• Intra articular steroids may be of temporary benefit in flar-ups (relieve pain for 2-6 weks), frequent injections in the same joint should be avoided.
• Intraarticular hyaluronic acid derivatives may be of value.
Surgery:
• Total joint replacement
• Osteotomy by arthroscope
• Osteoarthritis (osteoarthrosis) may be primary or secondary. Usually it is the end result of a variety of pattern of joint failure.
• It is characterized by degeneration of articular cartilage with simultaneous proliferation of new bone, cartilage and connective tissue leading to remodelling of joint contour, inflammation of synovial membrane is minor and secondary.
Risk factors of Osteoarthritis
1- Wear and tear. 2- Aging.
2- Aging.3- Genetic factors.
4- Obesity (loading stress on weight
bearing joint e.g. knee).
5- Smoking
Pathogenesis of Osteoarthritis
1- Matrix loss is due to release of proteases and collagenases. The interleukin I and TNF are the mediators of these catabolic effects, also these cytokines leading to synovial inflammation.2- Growth factors e.g insulin like growth factor and transforming growth factor are involved in stimulating collagen repair and production of the over growth at the joint margin (osteophytes).
• Cartilage is a matrix of collagen fibres enclosing a mixture of proteoglycans and.water .
• Under normal circumstances there is a dynamic balance between cartilage degradation by wear and its production by chondrocytes.
• Early, in cases of osteoarthritis the cartilage becomes fissured and ulcerated due to collagen matrix breakdown.
• Cartilage ulceration exposes underlying bone to increased stress producing rnicrofractures and cysts.
The bone attempts repair but produces abnormal sclerotic subchondral bone and over growth at joint margin called osteophytes.
Classification ( Types ) of Osteoarthritis
1- Primary osteoarthritis:• Localized.
• Generalized (3 or more joint areas)
2- Secondary osteoarthritis :-
• Mechanical e.g. occupational, hypermobility, cruciate tears.
• Metabolic: Haemochromatosis, Wilson's disease.
• Inflammatory: Rheumatoid arthritis, Gout, sero-ve arthropathy.
• Developmental: Epiphyseal dysplasia.
• Miscellaneous: Haemophilia, neuropathies.
Clinical picture of Osteoarthritis
patient over age 45 and often over age of 60Symptoms
Osteoarthritis affects many joints with insidious onset. Hip and knee osteoarthritis is the major cause of disability.
1- Pain (progressive i.e. months to years) which worsens with activity and is relived by rest.
2- Morning stiffness (brief < 15 minutes).
3- Gelling phenomenon refers to the sense of renewed stiffness in diseased joint after prolonged inactivity
Signs
1- Tenderness with limitation of range of movement (capsular thickening, blocking by osteophyte).
2- Crepitus on movement due to rough articular surfaces.
3- Joint enlargement due to soft tissue swelling or osteophytes.
4- Deformity e.g - Varus (medial angulation) , valgus (lateral angulation)
5- Joint effusion, wasting of muscles.
6- Osteoarthritis of the hands leading to:
• Heberden's nodes: Bony swelling of distal inter-phalyngeal joint.
• Bouchard's nodes: Bony swelling of proximal inter-phalyngeal joint.
Investigations to diagnose Osteoarthritis
• Blood picture ESR, and eRP are normal.• Rheumatoid factor and ANA are nagative
• X ray - Joint space narrowing (loss of cartilage).
- Marginal osteophytes.
- Subchondral sclerosis.
• MRI Showing early cartilage changes
• Arthroscopy can reveal surface erosion and fissuring of the cartilage.
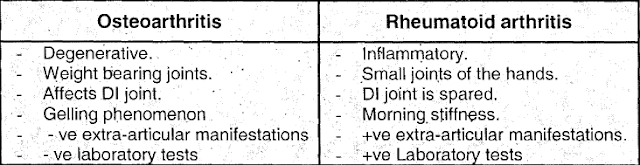
Differential diagnosis of Osteoarthritis
Treatment of Osteoarthritis
Non pharmacologic treatment:• Weight loss, joint rest.
• Knee cage, cervical collar or lumbar corset.
• Exercise to support muscle around joint (the best is swimming), strengthening exercises for quadriceps.
• Heat modalities.
Pharmacologic therapy:
• Topical NSAIDs are safe and relatively effective.
• Oral paracetamol 1gm TDS and when needed, it is safe and welltolerated.
• Oral NSAIDs are more potent than paracetamol but they may lead to gastritis, peptic ulcer, nephrotoxicity.
• Oral glucosamine sulphate, may have chondroprotective effect.
• Intra articular steroids may be of temporary benefit in flar-ups (relieve pain for 2-6 weks), frequent injections in the same joint should be avoided.
• Intraarticular hyaluronic acid derivatives may be of value.
Surgery:
• Total joint replacement
• Osteotomy by arthroscope