Characters of the genus Staphylococcus:
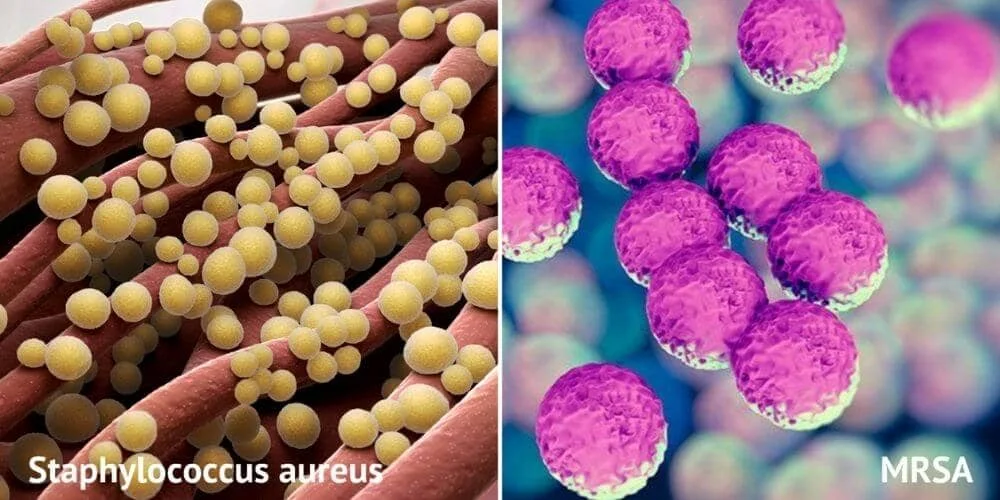
- Gram-positive spherical cocci arranged in grape-like clusters. (Fig. 1)
 |
| Fig. 1: Staphylococci in culture |
- Catalase positive. (Fig. 2)
 |
| Fig. 2: Catalase test positive |
- Opaque, pigmented colonies are usually produced on agar.
The ability to produce staphylocoagulase divides the genus into two groups: (Fig. 3)
- Coagulase-positive staphylococci: S. aureus has the greatest pathogenic potential and is the most medically important species.
- Coagulase-negative staphylococci: e.g., S. epidermidis and S. saprophyticus which are far less pathogenic.
 |
| Fig. 3: Coagulase test |
Morphology
S. aureus strains, like other staphylococci, are Gram-positive spherical cocci (about 1 μm in diameter) occurring in irregular grape-like clusters.
Cultural characters
- S. aureus is a facultative anaerobe.
- It usually produces golden yellow endopigment. (Fig. 4)
 |
| Fig. 4: Staph. aureus on nutrient agar |
It is usually grown on:
- Blood agar, producing complete (β) haemolysis due to production of haemolysins. (Fig. 5)
 |
| Fig. 5: Staph aureus on blood agar with complete beta hemolysis |
- Nutrient agar.
- Mannitol salt agar (selective indicator medium) producing yellow colonies due to mannitol fermentation. This medium facilitates isolation of S. aureus (salt tolerant) from specimens contaminated by other bacteria. (Fig. 6)
 |
| Fig. 6: Staph aureus on mannitol salt agar (Yellow colonies) |
Virulence factors and pathogenesis
1. Staphylocoagulase: Coagulase is an extracellular protein that has the ability to convert plasma fibrinogen to fibrin. By this mechanism, a fibrin barrier is formed.
This leads to:
- Protection from phagocytic and immune defences.
- Localization of infection in tissues e.g., furuncles.
2. The clumping factor (fibrinogen-binding protein): This is an important adhesin that leads to attachment of the organism to traumatized tissue and blood clots.
3. Invasins: Leucocidin, staphylokinase and hyaluronidase promote bacterial spread in tissues.
4. Protein A: It is present on surface of S. aureus. It binds non-specifically to the Fc-portion of IgG leading to inhibition of opsonization. (Fig. 7)
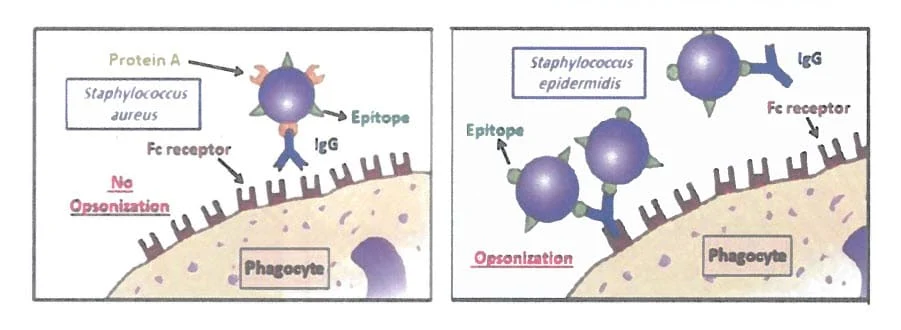 |
| Fig. 7: Role of protein A virulence factor |
5. Haemolysins (e.g. alpha toxin): These are pore-forming toxins that lyse host
cell membranes. They cause haemolysis on blood agar.
6. Exotoxins having superantigen mechanism.
a- Enterotoxins responsible for staphylococcal food poisoning.
b- Toxic shock syndrome toxin-1 (TSST-1).
c- Epidermolytic (exfoliatin) toxins responsible for staphylococcal scalded skin syndrome (SSSS).
Staphylococcus aureus Diseases
Staphylococci usually inhabit the skin (especially the perineum) and mucosa. The nose is the main habitat for S. aureus with a nasal carriage rate of more than 40% in adults.
The chief sources of infection are shedding human lesions, fomites contaminated from such lesions, the human respiratory tract and skin.
Contact spread of infection is of significant importance in hospitals, where a large proportion of the staff and patients carry antibiotic-resistant staphylococci in the nose or on the skin.
Contaminated hands of the healthcare workers account for transmission of several healthcare-associated infections.
A. Pyogenic diseases
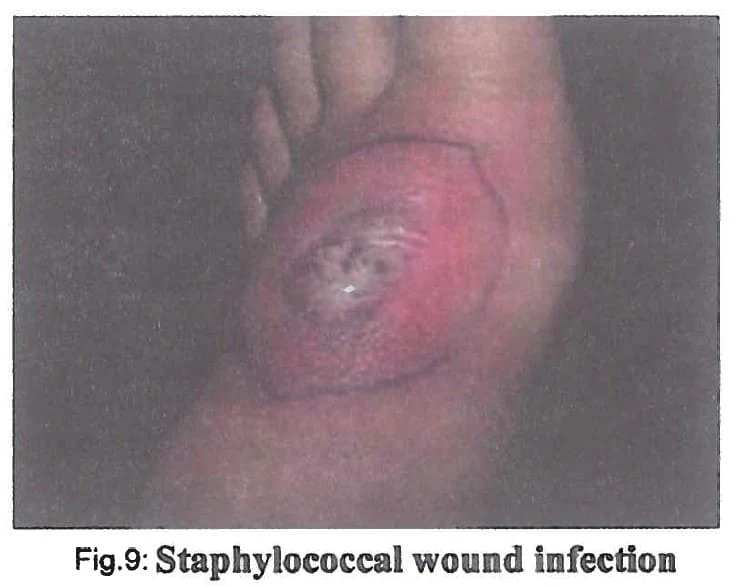
I. Localized skin infections are by far the most common. (Fig. 8 & 9)
- Folliculitis, furuncles, carbuncles, or abscesses.
- Surgical site infections.
- Traumatic wound infections following skin injury and burns.
II. Staphylococcal pneumonia is a frequent complication of prior viral infections (e.g. measles or influenza).
III. Invasive conditions are more serious and usually occur in immuno-compromised individuals.
Invasion of bloodstream (bacteraemia) and spread to numerous body sites lead to deep seated infections such as osteomyelitis, endocarditis and meningitis. A resulting septicaemia may be rapidly fatal.
B. Toxin-mediated diseases
I. Staphylococcal food poisoning:
It is the commonest type of bacterial food poisoning.
Incriminated foods include protein-rich food like mayonnaise, milk and its products (e.g. ice cream), or carbohydrate-rich food e.g. pasta, cake and koskosi.
The source of food contamination may be:
- A carrier such as food handlers harbouring S. aureus on their hands or in the nose.
- A person with pyogenic staphylococcal infection e.g., furuncle.
The organism grows in the food and produces the toxin.
There are at least six antigenic types of enterotoxins (A, B, C, D, E and G) produced by ~50% of S. aureus strains. These toxins use a superantigen mechanism.
Staphylococcal enterotoxins do not change the characteristics of the food, regarding its taste, color, or odor.
In addition, heating may kill the organism, but does not destroy the toxin since it is heat-stable (for ~30 minutes of boiling).
Incubation period is characteristically short (1-6 hours after ingestion of foods containing preformed toxin).
It manifests as violent vomiting and diarrhoea, usually without fever.
It is usually self-limited.
II. Toxic shock syndrome (TSS)
TSS is due to infection or colonization by TSST1-producing S. aureus.
It was first described in young menstruating females who use vaginal tampons that are left in place for extended period. However, the syndrome can also occur in any individual suffering from TSST-1 producing S. aureus infections anywhere in the body.
The disease is characterized by sudden onset of high fever, diarrhoea, vomiting and red rash.
Hypotension with cardiac and renal failure may occur due to the superantigen action of TSST-1.
The mortality rate may reach 10-15%.
III. Staphylococcal scalded skin syndrome (SSSS)
It occurs in neonates and children under 5 years of age.
It follows infections caused by S. aureus that produces exfoliatin toxins.
Large bullae are formed under the epidermis, which rupture leaving moist, red, scalded dermis.
Full recovery without scar formation is the rule.
 |
| Fig. 10: Staphylococcal scalded skin syndrome |
Laboratory diagnosis
a. Specimens: may include pus, sputum, urine, CSF or blood (in cases of bacteremia, septicemia and endocarditis), ....etc.
b. Direct Detection in Gram-stained smears: Gram-positive cocci are seen in clusters in association with pus cells.
Microscopy cannot discriminate staphylococcal species. (Fig. 11)
 |
| Fig. 11: Staphylococci in pus (Gram stain) |
c. Cultivation
- Specimens other than the blood should be plated directly onto blood agar and mannitol salt agar and incubated at 37°C.
- Blood samples should be cultivated by the blood culture technique. Subcultures are plated on blood agar and incubated as above.
d. Identification
After 24h incubation, the growth should be examined for colony morphology, Gram stain and catalase production. S. aureus is identified as follows:
- On blood agar: golden yellow colonies surrounded by complete haemolysis.
- On mannitol salt agar: yellow colonies.
- Gram-stained film: Gram positive cocci in clusters.
- Catalase test: positive.
- Coagulase test: positive. (Fig. 12)
- Test for the clumping factor: positive. (Fig.13)
Coagulase and clumping factor are the most important markers for identifying S. aureus in the laboratory.
In case of food poisoning:
Specimens: food remnants, vomitus and/or faeces should be tested for the causative S. aureus and/or its enterotoxin.
Isolation: on selective media such as mannitol salt agar as the specimens are usually contaminated with other bacteria.
Detection of enterotoxin production by the isolated strains or directly in the sample is done by ELISA.
In case of toxic shock syndrome:
The diagnosis usually depends on:
- Clinical findings.
- Isolation of the organism from suspected sites e.g., wounds, vagina or from tampons by culture on mannitol salt agar.
- Detection of TSST-1 in the blood by ELISA.
N.B.: Strain typing is required in the epidemiologic studies of outbreaks of S. aureus diseases such as food poisoning and surgical site infections.
Strain typing can be done by Colony morphology, Biotype profiles, Phage typing, Plasmid analysis, Ribotyping, Chromosomal analysis and PCR. (Fig.14)
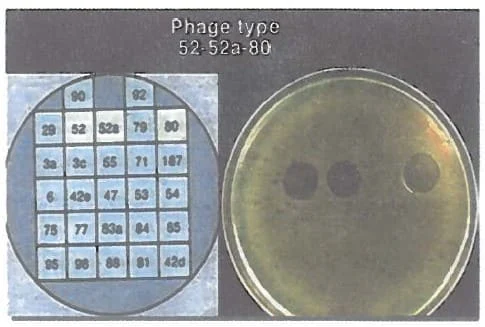 |
| Fig. 14: Phage typing |
Prevention and Control
Improved hygiene and proper infection control practices in hospitals are the most effective methods of prevention, especially hand hygiene and meticulous attention to aseptic techniques.