This is an approach to treatment of Pulmonary tuberculosis , with illustration of Drug doses , side effects, recommended course and possible combinations.
We are going to discuss the differential diagnosis (DDx) of tuberculosis
We are going to discuss the differential diagnosis (DDx) of tuberculosis
A. Medical (Drug) treatment of Tuberculosis
1- Bed rest and isolation of patients who are excreting the organism
2- Good nourishment
3- Drugs:
Rules
1- Long course to avoid relapse
2- Combinations to avoid resistance (at least two antimicrobial agents)
3- Rifampicin shortens the course of treatment to 9 months.
4- I N H must be used
5- Side effects of drugs must be known.
Drugs
• I.N.H: the most effective constant drug, it is bactericidal, it interferes with lipid and nucleic acid synthesis.
Dose: 200-300 mg/day (5mg/kg)
Side effects: hepatotoxicity, polyneuropathy. Pyridoxine 10 mg/d is given to prevent polyneuropathy.
INH is acetylated in the liver, so rapid acetylators are more liable to develop hepatitis
due to the acetylated metabolite, however slow acetylators are more liable to
develop neuropathy.
• Streptomycin (Bactericidal):
- Dose: 1gm I.M daily
- Main side effects: ototoxicity ( irreversible)
• Rifampicin (Bactericidal, it inhibitis DNA dependent RNA polymerase) (10 mg/kg).
450-600 mg/d, it is hepatotoxic, it also causes vasculititis, hypersensitivity nephritis and flu like symptoms.
• Ethambutol ((Bacteriostatic inhibiting RNA synthesis)
10-25 mg/kg, it leads to optic neuritis
• Pyrazinamid (PZA) (Bactericidal)
20- 30 mg/kg, (It may lead to hepatitis and hyperuricemia)
B. Surgical ttt
Lobectomy with resistant cases or recurrent haemoptysis.
Role of corticosteroids. In cases of T.B
Indications :
1- Miliary T.B
2- Serous membrane affection to prevent fibrosis.
3- Replacement therapy if it leads to Addison's disease .
• Chemo prophylaxis of T.B
INH for 6-12 months or INH and rifampicin for 3 months or pyrazinamid and rifampicin for 2 months can be given in non vaccinated contact who have recently
tuberculin +ve, or in immunosuppressed contacts regardless the result of tuberculin.
Infants of highly infectious mothers given in INH 5 mg/kg/d for 6 weeks.
Opinion:
• Tuberculin negative contacts, especially children should receive prophylaxis for 2-3 months and should be retested with tuberculin. Those whose results remain negative should discontinue prophylaxis.
• Contacts immunocompromised patients especially HIV patients and organ transplant recipients should receive a full course of treatment regardless the tuberculin results !?
# BCG (Bacille calmette - Guerin) (Attenuated M. bovis).
0.1 ml l.D at the junction of the upper and middle 1/3 of the upper arm. Its protective efficacy is up to 80% for 10-15 years and is greatest for preventing disseminated disease in children. It should not be used when there is known immunodeficiency. Tuberculin test can become positive after BCG administration.
Recent antituberculous can be used in resistant cases of tuberculosis
• Capreomycin • Cycloserine
• Clarithromycine • Azithromycine
• Ciprofloxacine • Ofloxacine.
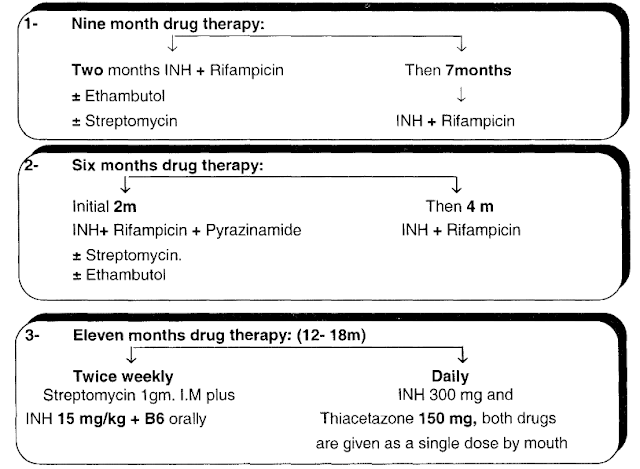
Protocols or regimens of treatment of Tuberculosis
Important notes
• Pregnant patients should be treated as usual but PZA, streptomycin must be avoided.
• Patients with chronic liver disease can receive the usual treatment except (rifampicin), smaller dose of INH can be used.
• Patients with chronic renal failure can receive INH and rifampicine with the usual dose.
• Response to empirical antituberculous drugs usually seen after 1-2 weeks, this can be used as a therapeutic test for diagnosis of tuberculosis.
• Continued symptoms or persistently positive smears or cultures after 3 months of treatment should raise the suspicion of druq resistance or non compliance.
2- Cases with bronchopneumonia
3- Mediastinal lymph node enlargement e.g. sarcoidosis or lymphoma.
4- Coin shadow in chest x ray • Bronchial carcinoma, Bronchial adenoma
5- Miliary shadows in chest x ray
6- Fever of unknown etiology.
Important links to related articles
-Pulmonary Tuberculosis def., causes, risks, pathology
- Manifestations of Pulmonary Tuberculosis (symptoms, signs)
- Miliary tuberculosis manifestations and investigations
- Complications of pulmonary tuberculosis
- Tuberculosis diagnostic investigations and Tuberculin test
• Patients with chronic liver disease can receive the usual treatment except (rifampicin), smaller dose of INH can be used.
• Patients with chronic renal failure can receive INH and rifampicine with the usual dose.
• Response to empirical antituberculous drugs usually seen after 1-2 weeks, this can be used as a therapeutic test for diagnosis of tuberculosis.
• Continued symptoms or persistently positive smears or cultures after 3 months of treatment should raise the suspicion of druq resistance or non compliance.
Differential diagnosis (DD) of T.B
1- Cases of pleural effusion2- Cases with bronchopneumonia
3- Mediastinal lymph node enlargement e.g. sarcoidosis or lymphoma.
4- Coin shadow in chest x ray • Bronchial carcinoma, Bronchial adenoma
5- Miliary shadows in chest x ray
6- Fever of unknown etiology.
Important links to related articles
-Pulmonary Tuberculosis def., causes, risks, pathology
- Manifestations of Pulmonary Tuberculosis (symptoms, signs)
- Miliary tuberculosis manifestations and investigations
- Complications of pulmonary tuberculosis
- Tuberculosis diagnostic investigations and Tuberculin test