Definition: Rhinitis is defined clinically by a combination of two or more nasal symptoms: running nose, blocking, itching, and sneezing. Allergic rhinitis occurs when these symptoms are the result of IgE-mediated inflammation, following exposure to allergen.
Etiology (Causes, predisposing and exciting factors)
(A) Predisposing factors:
- Genetic predisposition: it is the best established risk factor, gene involved in atopy include loci on 5q, 11q, and 12q.
- Living in developed countries, pollution, climate interaction, and good hygiene, all seem to be risk factors.
(B) Exciting factors:
The globally important allergens are: house dust, mites, grass, tree and weed pollen, pets, cockroaches and moulds.
Incidence:
Quoted provenance figures vary widely from 1 to 40%.
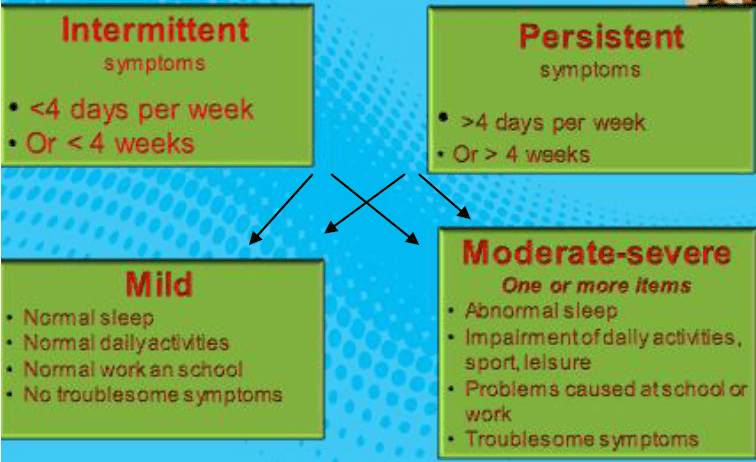
May be: seasonal, perennial, or mixed.
Classification:
Pathogenesis: type I hypersensitivity
- Sensitization: allergen is captured by Langerhans cells……stimulate IgE production by B cells.
- Subsequent reaction to allergen (early phase), with release of mediators like histamine, leukotrienes, prostaglandins, and C4, causing sneezing, itching, rhinorrhea, and nasal block.
- Late phase reaction: in half of patients, involves the ingress of eosinophils, basophils, mast cells, T lymphocytes, neutrophils, and macrophages to tissues.
Pathology:
- Edema.
- Infiltration with eosinophils & plasma cells.
- Watery discharge with high serous content.
- Vascular dilatation, stasis leads to purple color.
- Polypi: pedunculated edematous mucosa.
- Superadded infection: red mucosa and viscid discharge.
Symptoms:
- Nasal itching & sneezing.
- Bilateral watery discharge may be postnasal drip.
- Bilateral or alternating nasal obstruction.
- Anosmia, continuous or intermittent.
- Asthma: most asthmatics have rhinitis, and about one third of rhinitis patients have asthma.
Signs:
- Edematous pale blue mucosa.
- Excessive watery secretions.
- Swollen edematous turbinates.
- May be allergic nasal polypi.
- In children: allergic salute.
Investigations: Following history and examination
- Nasal cytology: eosinophilia.
- Skin prick testing
Technique: forearm skin is pricked with needle passed via diluted different allergens
Results: Positive…... Central wheel surrounded by erythema.
Value : Confirm suspected allergen …. In relation to history.
- Nasal challenge test.
Technique: Diluted aqueous extract sprayed in the nose
- Blood examination.
-Eosinophilia. -Increased total IgE.
-Increased plasma IgE level to specific Ag.
Treatment of Allergic rhinitis:
(A) Medical:
- Avoid exposure to offending antigen.
- Hypo sensitization (Immunotherapy) to form IgG (blocking antibodies).
- Mast cell stabilizers: sodium chromoglycate (spray 4-6 times daily).
- Antihistaminics: astemizole, loratadine, fexofenadine (oral or nasal spray).
- Steroids: topical, systemic, or depot. Topical steroids are considered the most effective treatment for rhinitis.
- Ipratropium bromide: useful against watery rhinorrhea.
- Nasal drops for short time to avoid rhinitis medicamentosa.
- Oral decongestants.
- Recently antineutrinos: effective against congestion and edema, useful in nasal polyposis.
(B) Surgical:
- Turbinate reduction.
- ESS, for sinonasal polyposis.
- Vidian neurectomy (rarely done now).