Antimicrobial chemotherapeutic agents: are chemically synthesized substances that are used to treat infectious diseases by killing or inhibiting the growth (or multiplication) of microorganisms.
Antibiotics: are low-molecular weight antimicrobial substances that are produced as secondary metabolites by certain groups of microorganisms, especially Bali Streptomyces, Bacillus, and a few moulds (Penicillium and Cephalosporium).
Although their original source was a microorganism, some antibiotics are currently made synthetically (synthetic antibiotics).
Chemical modification of certain antibiotics, to achieve the desired properties, has been a prominent method of new drug development (semisynthetic antibiotics).
Terminology
Bacteriostatic agent: is an antimicrobial agent that is capable of inhibiting bacterial multiplication. Multiplication resumes upon removal of the agent.
Bactericidal agent: is an antimicrobial agent that is capable of killing bacteria. Multiplication can not be resumed.
Selective toxicity: is the ability of an antimicrobial agent to harm a pathogen without harming the host. It may be a function of a specific receptor (or target) for the drug found in the microbe but not in the human body (e.g. peptidoglycan), or it may depend on the inhibition of a biochemical event essential for the organism but not for the host.
Spectrum of activity: the range of microorganisms that are affected by a certain antibiotic is expressed as its spectrum of action.
Antibiotics which kill or inhibit the growth of a wide range of Gram-positive and Gram-negative bacteria are said to be broad spectrum.
If effective mainly against either Gram-positive or Gram-negative bacteria, they are narrow spectrum.
If effective against a single organism or disease, they are referred to as limited spectrum.
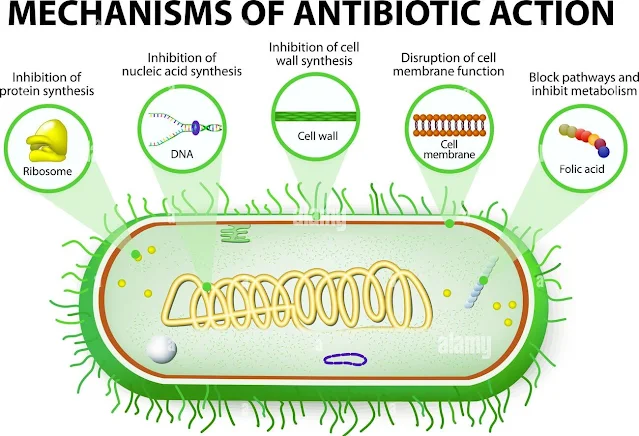
Mechanisms of Action of Antimicrobial Agents
There are four mechanisms by which an antimicrobial can eradicate an infection.
These mechanisms are:
A. Inhibition of bacterial cell wall synthesis
Agents acting by this mechanism include:
- Beta-lactam antibiotics: e.g. penicillins, cephalosporins, and others.
- Glycopeptides: e.g. vancomycin, and teicoplanin.
- Cycloserine and bacitracin.
These antibiotics are bactericidal with minimal tissue toxicity.
The B-lactam drugs inhibit the last steps of peptidoglycan synthesis. This inhibition is initiated by binding of the drug to certain cell receptors known as penicillin-binding proteins (PBPs).
On the other hand, glycopeptides and cycloserine inhibit early steps in the biosynthesis of peptidoglycan, which occur inside the cytoplasmic membrane.
Therefore, the mechanism of resistance to ß-lactam antibiotics is different from that for the other groups. Subsequently, vancomycin could be used successfully in infections caused by ß-lactam resistant staphylococci.
B. Interference with the cell membrane function
Some agents disrupt the cytoplasmic membrane and interfere with its function. These include:
- Antibacterial agents: e.g. polymyxin and colistin.
- Antifungal agents: e.g. amphotericin B, nystatin and imidazoles.
C. Inhibition of bacterial protein synthesis
Bacteria have 70S ribosomes (with 30S and 50S subunits) whereas mammalian cells have 80S ribosomes (40S and 60S subunits).
This difference makes bacterial ribosomes a selective target for antibiotics.
Agents acting on the 30S ribosomal subunit:
- Tetracyclines
- Aminoglycosides (gentamicin, amikacin, streptomycin)
Agents acting on the 50S ribosomal subunit:
- Macrolides (erythromycin, azithromycin)
- Lincomycins (clindamycin)
- Streptogramins
- Linezolid
- Chloramphenicol
- Fusidic acid
D. Inhibition of bacterial nucleic acid synthesis
This may occur by:
- Inhibition of RNA synthesis through the strong binding to DNA-dependent RNA polymerase: e.g. rifampin.
- Inhibition of DNA synthesis through blocking DNA gyrase: e.g. quinolones and novobiocin.
- Inhibition of dihydrofolic acid reductase leading to inhibition of folic acid synthesis. The latter is important for purine synthesis and, consequently, nucleic acid formation. Examples of these antimicrobials include trimethoprim and pyrimethamine.
- Inhibition of folic acid synthesis by competitive antagonism e.g. sulphonamides. For many organisms, para-amino benzoic acid (PABA) is essential for the synthesis of folic acid. Sulphonamides are structural analogues of PABA. They compete with PABA for the active centre of the enzyme involved in folic acid synthesis. As a result, nonfunctional analogues of folic acid are formed and nucleic acid synthesis is inhibited.
Choice of an Antimicrobial Agent for Therapy
The following are guidelines that can be followed for proper antibiotic use:
- Select an antibiotic that is able to penetrate to the site of infection and achieve effective concentration, e.g. certain drugs are able to pass the blood-brain barrier, others are highly concentrated in urine.
- Identify the nature of the infection whether bacterial, viral, fungal, or parasitic. A common mistake is to give an antibacterial agent for a viral infection.
- Choose as narrow an antibiotic spectrum as you can. When you get the results of culture and susceptibility, revise your treatment to 'narrow-down' the spectrum as far as possible. The use of broad spectrum antibiotics is likely to faster induce resistance to antibiotics and may be complicated by superinfection.
- Give the appropriate dose of the antibiotic for the proper duration. Inadequate dosage or undue prolonged therapy may result in drug toxicity and antibiotic resistance.
- Know the potential of the drug to produce toxicity: Some drugs known to be of low toxicity will exert high toxicity if they accumulate in the blood due to liver or kidney dysfunction. Use antibiotics that are only safe for the pregnant and lactating women and for infants and children.
- Choose bactericidal rather than bacteriostatic antibiotics.