Antibiotic resistance is a global problem faced today in the treatment of infectious diseases. Resistance to antibiotics is more prevalent in hospitals especially intensive care units due to the higher antibiotic use.
Resistance to antimicrobial agents is of two categories either Intrinsic or acquired.
Intrinsic resistance (inherent or natural)
This type of resistance refers to bacteria that are insensitive, in their natural state, to an antibiotic without the acquisition of resistance factors.
It is consistent and can be expected once the organism is known.
Intrinsic resistance occurs in the following situations:
- Streptomycetes are protected from the antibiotics they produce.
- Gram-negative cell membrane has pores too small to allow large antibiotic molecules, e.g. nafcillin, to penetrate.
- An organism lacks the target or receptor for the antibiotic as in the case of resistance of Enterococcus species to cephalosporins.
Acquired resistance
It results from altered bacterial physiology and structure due to changes in the genome of the organism. It is inconsistent and unpredictable.
The unpredictable nature of this resistance is the primary reason why laboratory methods to detect resistance are necessary.
Acquired resistance mechanisms are driven by two genetic processes in bacteria:
- Mutation and selection: Sometimes referred to as vertical evolution. Exposure of an organism to an antibiotic exerts a selective pressure on the organism and leads to mutation. The more frequent the exposure to the antibiotic the greater the potential resistance.
- Exchange of genes between strains and species: Sometimes referred to as vertical evolution. Resistance genes can be encoded on plasmids, phages and transposable genetic elements.
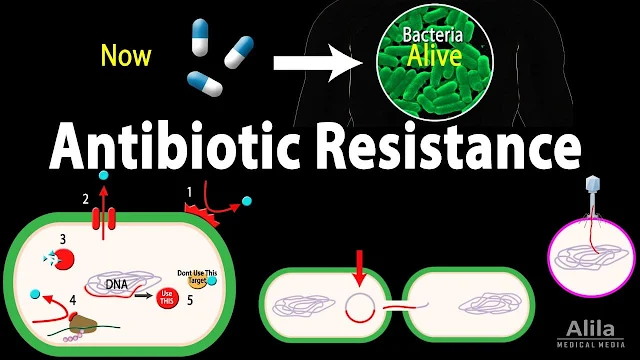
Mechanisms of Acquired Resistance
Bacteria have the ability to use one or more of the following mechanisms:
A) Reduction of the intracellular concentration of the antibiotic by:
1. Decrease in influx of antibiotic through:
- Reduction of permeability of the outer membrane by modification or
- Loss of porin (a hollow membrane protein) required for entry of the antibiotic molecules.
2. Efflux pumps:
The antibiotic is pumped out across the cytoplasmic membrane faster than it can diffuse in, so the
concentration of antibiotic remains too low to be effective.
B) Inactivation of the antibiotic, e.g.:
- Production of B-lactamases leads to hydrolysis of the B-lactam ring, thus inactivating penicillins and cephalosporins.
- Production of acetyl transferase results in chloramphenicol resistance.
- Production of aminoglycosides-modifying enzymes.
C) Target modification:
Modification of the target site for the antibiotic results in a reduced affinity for its receptor.
Examples:
- Modification of the penicillin-binding proteins (PBPs) is a primary mode of resistance to ß-lactam antibiotics in methicillin-resistant S. aureus (MRSA).
- Alteration of the 50S ribosomal subunit reduces the affinity of macrolides linezolid and streptogramins for the ribosome.
- Alteration of the 30S ribosomal subunit reduces the affinity of aminoglycosides for the ribosome.
D) Target elimination:
By developing new metabolic pathways: These have the ability to create new metabolic pathways that bypass the target, e.g. resistance to trimethoprim.
E) Target overproduction:
This may be the mechanism used by S. aureus strains with intermediate susceptibility to vancomycin (VISA).
Antimicrobial Chemoprophylaxis
The prevention of disease using antimicrobial drugs.
Antimicrobial chemoprophylaxis is the administration of an effective antimicrobial agent to prevent, rather than to treat, infection with a certain microbe, thus preventing development of a disease.
Examples of antimicrobial chemoprophylaxis include:
- Long-acting penicillin (or erythromycin) is given to rheumatic patients to prevent reinfection with S. pyogenes.
- Rifampicin is given to close contacts of meningococcal meningitis for 2 days to prevent meningitis.
- Penicillin or erythromycin is given to individuals with abnormal heart valves prior to dental procedures to prevent endocarditis.
- Antibiotics are given prior to some surgical operations to prevent infection.
- Antimicrobial chemoprophylaxis should only be used when the risk of infection is high and the benefits of prophylaxis outweigh the risks.
Antimicrobial resistance is a serious public health threat. It is important to use antibiotics judiciously to prevent the development and spread of resistance.