Definition:
Fibrocystic breast disease refers to benign (noncancerous) changes in the tissues of the breast.
The term "disease" in this case is misleading, and many health care providers prefer the term "change".
The condition is so common that it is believed to be a variation of normal.
Other names:
- ANDI: abbreviation for "Aberration in Normal Development and Involution of the breast".
- Fibrocystic disease of the breast.
- Sector mastitis.
- Mammary dysplasia.
- Chronic interstitial mastitis: misnomer as in this condition there is no evidence of inflammation.
Incidence:
- The most frequent breast disorder (it occurs after puberty and before menopause).
- Most common between 30-50 years old
Etiology (unknown):
1. The breast undergoes changes throughout the woman's reproductive life with cyclic changes during the menstrual cycle. The high prevalence of the disease in women in child bearing period points to a relation to ovarian cycle.
2. Other Factors:
- High unopposed estrogen level with abnormal breast response
- High Prolactin levels
- Viral infection
Pathology
The upper outer quadrant of the breast is the commonest site of affection.
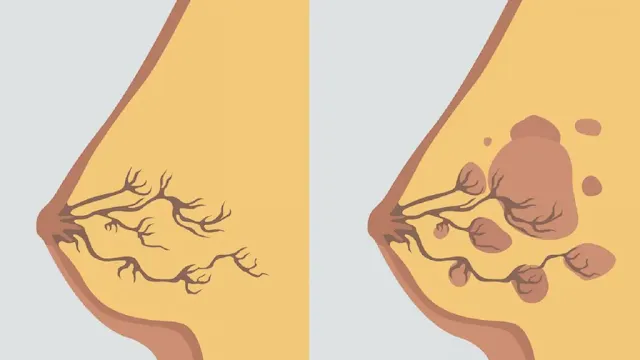
It is characterized by:
- Adenosis: Glandular hyperplasia with increased number acini.
- Fibrosis: fibrous tissue replaces elastic & fatty tissue.
- Fibrosis leads to duct obstruction which results in "retention cyst" formation.
- It may be unilateral or bilateral or affecting a sector of breast
- Epitheliosis: Epithelial hyperplasia in small ducts.
- Extensive epitheliosis: intra-ductal papillary growth which is termed papillomatosis
- Rarely, there's "Atypical epithelial hyperplasia": precancerous
- Extensive fibrosis may resemble schirrous carcinoma & called "sclerosing adenosis"
- Round cell infiltration.
- Cyst formation: The cyst might be small (microcyst) or large (macrocyst).The cysts may coalesce to form (blue domed cyst of Bloodgood): A large cyst contains altered blood.
It is NOT Precancerous.
Most of the surgeons consider the fibroadenosis not precancerous, Except if there is marked papillomatosis or atypical epithelial hyperplasia.
Hyperplasia and papillomatosis increase risk of malignancy 1.5-2 times but atypical hyperplasia increases the risk of malignancy 5 times.
Clinical Picture
Type of patient: It occurs after puberty or before menopause, multiple painful lumps that may be unilateral or bilateral and it is related to menstrual cycle.
Symptoms:
It may be completely asymptomatic.
The following changes are usually CYCLIC:
1. Breast pain (Mastalgia. Mastodynia):
- Exaggerated pre-menstrual tension
- Dull aching or stitching pain
- Increased Pre-menstrually & by breast movement & Decreased post-menstrually & by breast support.
- Associated with enlargement and increased nodularity of breast
2. Breast lump (Cysts or sclerosing adenosis):
- The Most frequent complaint
- May disappear when the patient is re-examined 1 week after menstrual cycle
3. Breast discharge:
- Usually clear or yellow
- Sometimes brown or green
Local Examination:
1. Breast Lump:
- May be solid or cystic, freely mobile, commonly bilateral and diffuse. .
- Better to be felt by tip of fingers not by flat of the hand (painful nodularity).
2. Discharge:
- With gentle squeeze.
- Colorless fluid or greenish discharge.
3- Axillary Lymph Nodes:
May be elastic, enlarged, tender and mobile with shotty distribution.
Non-cyclic Mastalgia
- It may be associated with ANDI or with periductal mastitis.
- It is more common in premenopausalfemales than postmenopausal.
- It should be differentiated from referred pain as musculoskeletal disorders.
- Breast pain in postmenopausal women not taking hormone replacement therapy is usually derived from chest wall.
Complications
- Increased risk of malignancy, only if marked epitheliosis and papillomatosis.
- Hemorrhage and infection in cyst of Bloodgood.
- Anxiety (if severe pain).
Differential diagnosis
1. Breast pain:
- Premenstrual tension.
- Malignancy (if advanced or mastitis carcinomatosis)
- Inflammation
2. Breast lump:
- Fibro-adenoma.
- Breast carcinoma. (The most dangerous).
3. Breast discharge:
- Duct ectasia (the commonest).
- Fibroadenosis.
- Duct papilloma (the commonest cause of bloody discharge).
- Duct carcinoma.
- Galactorrhea of pituitary adenoma.
Investigations
Treatment of Fibro-adenosis
Reassurance of the patient from cancer phobia is the most important.
a. Changing life style
- Firm bra.
- Avoid coffee, tea and chocolate.
- Regular intake of 400 IU of vitamin E may be helpful.
b. Medical treatment
- Analgesics
- Regulation of the cycle.
- Prim-rose oil single evening dose.
- Parlodel 2.5 mg tab/twice /day (anti-prolactin).
- Danazol tab!!! (last line of TTT as it causes acne & hirsutism)
- Psychotherapy
c. Indications of surgery
- Biopsy: if doubtful diagnosis.
- Excision of the cyst: large cyst (cyst of Bloodgood).
- Cysts are treated by asplration; recurring cysts, sclerosing adenosis or any cancer doubt are excised for biopsy.
Cases with atypical epithelial hyperplasia (discovered by biopsy) should be instructedto perform breast self examination monthly, physical examination every 3-6 months &mammography yearly.
Prognosis
Exacerbations may occur at any time until the menopause except in patients who receive hormonal replacement therapy.
Summary
- Fibroadenomas are painless, unilateral, benign (non-cancerous) breast tumors that are solid, not fluid-filled, lumps.
- They occur most commonly in women between the ages of 14 and 35 years, but can be found at any age.
- Fibroadenomas are caused by hormonal changes, and they tend to shrink after menopause.
- Fibroadenomas are diagnosed with a mammogram or ultrasound, and they may be biopsied to confirm the diagnosis.
- Most fibroadenomas do not need treatment, but they may be removed if they are large or if they are causing pain.
- The prognosis for fibroadenomas is excellent.