Any individual is protected from potentially harmful microorganisms in the environment by a number of very effective mechanisms present since birth.
They do not depend upon prior exposure to any particular microorganism. They are non-specific and can act against any microorganism or foreign invader.
Mechanisms of Innate Immunity include:
I. Natural mechanical barriers and surface secretions
- Intact skin and mucous membranes constitute a barrier that cannot be penetrated by most microorganisms.
- The sticky mucus covering mucous membranes traps any foreign material.
- Cilia of the respiratory tract epithelium sweep foreign material out.
- Blinking, sneezing and coughing reflexes expel foreign particles.
- The flushing action of saliva, tears and urine helps in washing microbes from the body.
- Sweat and sebaceous secretions contain substances (e.g. lactic acid and ammonia) that inhibit microorganisms.
- Saliva, tears and mucous secretions of respiratory, alimentary and genitourinary tracts contain lysozyme which is bactericidal.
- Gastric and vaginal acidity inhibit growth of microorganisms.
 |
| Fig. 1: Natural mechanical barriers |
II. Normal bacterial flora
- Bacteria of the normal flora produce bacteriocins and acids that destroy microorganisms.
- They compete with pathogens for essential nutrients.
N.B.: Suppression of normal flora by antibiotics may lead to infection with potential pathogens (superinfection).
III. Soluble defense factors
A number of microbicidal substances are present in tissues and body fluids and act in
defence against microbes. They include:
1. Lysozyme: It is an enzyme that lyses bacteria by destroying the peptidoglycan of
their cell wall.
2. Complement: It is a group of plasma proteins that act together to attack extracellular pathogens.
The complement components are present in an inactive form, and can be activated either spontaneously by certain pathogens (where it is considered to be part of innate immunity) or by antibody binding to the pathogen (where it is considered to be part of acquired immunity).
3. Acute phase proteins: These are present at very low levels in normal serum, but their concentration rises dramatically, shortly after the onset of an infection.
Microbial products, e.g. endotoxins, stimulate macrophages to release cytokines, which stimulate the liver to produce a large number of acute phase proteins.
These proteins limit the spread of the infectious agent or stimulate the host response. Examples include fibrinogen and C-reactive protein (CRP).
4. Interferons: There are 2 types of interferons. Type I interferon (alpha and ẞeta) is part of innate immunity.
It is secreted by virus-infected cells and prevents viral replication in uninfected neighboring cells (i.e. it 'interferes' with viral replication).
N.B.: Type II (omega) Interferon is secreted mainly by T cells, and is considered part of the acquired immune response.
 |
| Fig. 3: Humoral Innate immunity |
IV. Cellular defense factors
1. Phagocytes:
Particles, e.g. bacteria, entering the tissue fluids or blood are rapidly engulfed by phagocytic cells. This process of engulfment (internalization) of particulate matter is termed phagocytosis.
Phagocytes contain digestive enzymes capable of degrading ingested material.
The main phagocytic cells are:
- Neutrophils
- Monocytes/macrophages (monocytes in the blood and macrophages in the tissues)
- Dendritic cells
Stages of Phagocytosis
Phagocytosis occurs in subsequent steps:
a. Migration (Chemotaxis):
Microorganisms and injured tissues elaborate chemotactic factors that attract phagocytic cells to the site of infection.
Some of the complement components and some cytokines may have chemotactic properties.
b. Attachment:
Phagocytes have receptors on their surface that can recognize non-specific molecules common to many pathogens, allowing attachment to them.
Some microorganisms may alter these molecules or cover themselves with a thick capsule that is not recognized by any phagocyte receptor.
Attachment may still occur if these microorganisms become coated with molecules which the phagocytes can recognize.
These may be an antibody, a complement component or other molecules (e.g. CRP). In this case, the process is called opsonization and the substance which helped phagocytosis is called an opsonin.
c. Engulfment:
The cytoplasmic membrane of the phagocyte surrounds the organism and encloses it in vacuole termed phagosome.
Lysosomes, which are the bags of enzymes, then fuse with the phagosome forming phagolysosomes, in which the engulfed material is killed and digested.
d. Killing
This occurs via 2 mechanisms:
- Oxygen-dependant mechanism: After engulfment, there is a respiratory burst consisting of a steep rise in Oxygen consumption. This is accompanied by an increase in the activity of a number of enzymes and leads to generation of various reactive Oxygen intermediates, such as Hydrogen Peroxide and singlet Oxygen, which are lethal to micro-organisms.
- Oxygen-independant mechanism: These are the lysosomal enzymes (Lysozyme, Elastase, Hydrolase, .... etc.).
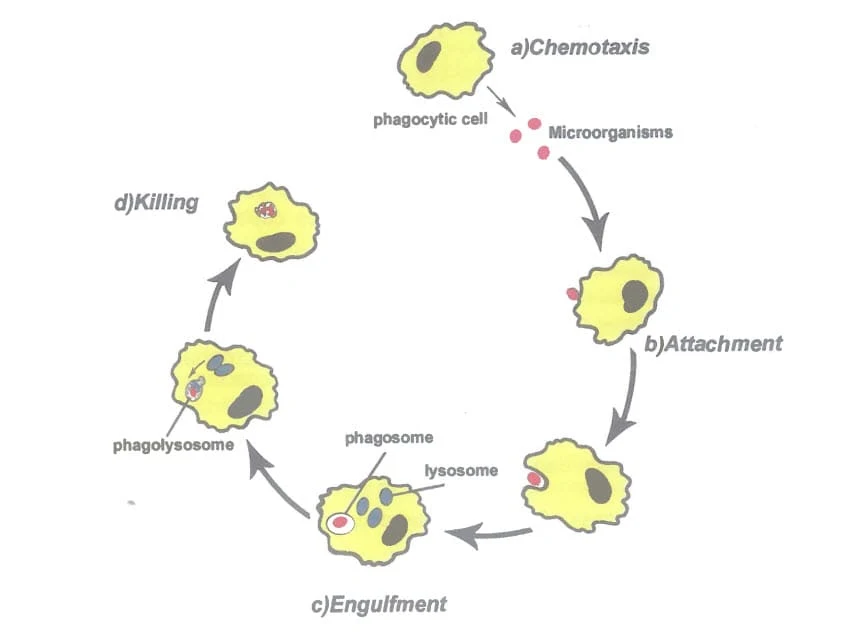 |
| Fig.4: Stages of Phagocytosis |
N.B.: In addition to phagocytosis, Monocytes and Macrophages have the following functions:
- Antigen presentation: Macrophages help to 'show' or 'present' part of the foreign agents they have eaten to T cells, so that the T cells can start responding to them. Thus, they are among a group of cells called antigen presenting cells (APCs).
- Secretion: They secrete chemical mediators called cytokines, e.g. interleukins.
- Direct cytotoxicity: They may kill targets without engulfing them. Helminthic parasites which are too large to be engulfed can be killed by macrophages releasing their toxic contents onto them. Tumour cells can also be killed in a similar way.
| Feature | Neutrophils | Monocytes/Macrophages |
|---|---|---|
| Importance | Most numerous and most important cells of the innate immune system | In addition to phagocytosis, have other important functions |
| Count | 60-80% of TLC* | 1-5% of TLC |
| Presence in normal tissues | Absent | Continuously leave the blood to the tissues where they mature into macrophages |
| Response during inflammation | Rapid increase in production | Slight increase in blood levels, slowly form granuloma, rapidly form pus |
| Size | Small | Large |
| Life-span | Short: die after phagocytosis, forming pus cells | Long: survive after phagocytosis |
| Functions | Phagocytosis | Phagocytosis, antigen presentation, cytokine secretion, direct cytotoxicity |
TLC = Total leucocytic count.
2. Eosinophils:
They are granulocytes present mainly in tissues. Count: In the blood, they form 1-3% of TLC.
Functions:
- They are mainly of importance in defence against helminthic parasite infections. Such parasites, which are too large to be phagocytosed, can be killed by eosinophils releasing the toxic contents of their granules onto them.
- They also play an important role in allergic reactions.
- Eosinophils also have phagocytic properties.
3. Basophils and mast cells:
• Basophils are found in the blood in very low concentrations (0-2% of TLC).
• Mast cells are their tissue resident form. They are present either around the blood vessels or in the submucosa.
Functions:
Both basophils and mast cells have similar functions.
They possess granules containing a number of important mediators such as histamine.
Release of these mediators:
- Contributes to inflammation
- Plays an important role in allergy
4. Natural killer cells
• They are large granular lymphocytes which can be distinguished from B and T lymphocytes.
Count: They constitute 10-15% of peripheral blood lymphocytes.
Functions:
- They are capable of non-specific killing of tumour cells and virus-infectednncells in a manner similar to cytotoxic T cells; however, they differ from cytotoxic T cells in the way they recognize their targets.
- They secrete cytokines such as interferon Gama.
The text in the image you sent is:
V. Inflammation
Chemical mediators released at the site of infection trigger an inflammatory response.
The events that occur during inflammation are vasodilatation, increased vascular permeability and migration of leucocytes from the blood stream across the vascular endothelium into the inflamed tissues to combat the invading microbe.
This migration is mediated by certain molecules, termed adhesion molecules, which are expressed on the surface of leucocytes and vascular endothelium.
N.B.: There is a lot of cooperation between innate and acquired immunity.
Examples:
- Innate immunity (macrophage) helps acquired immunity (T cell) through antigen presentation.
- Acquired immunity (antibody) helps innate immunity (macrophage) through opsonization.

