Pain is an unpleasant sensory and emotional experience for protection of the body.
It occurs whenever there is physical or potential tissue damage.
It causes the person to react to remove the pain stimulus or seek medical advice.
Pain Receptors
Types of Pain Receptors (Nociceptors):
Pain receptors are Free Nerve Endings attached to Aδ and C fibers.
They are classified according to the mode of stimulation into:
- Mechanical pain receptors: stimulated by mechanical injurious stimuli, e.g. cuts, bruises.
- Thermal pain receptors: respond to extremes of temperature and capsaicin (a substance present in hot chilli).
- Chemical pain receptors: stimulated by chemical injurious elements or chemicals produced from tissue damage.
- Polymodal pain receptors: respond to all types of stimuli.
Distribution of Pain receptors:
They are most numerous in superficial layers of the skin.
They are also numerous in peritoneum, pleura, periosteum, joints, arterial walls, dura and tentorium of the cranial cavity.
They are less distributed in deep tissues and very few in Internal viscera.
They are absent in liver parenchyma, lung (alveoli), and brain tissue (pain insensitive structures).
Adaptation: slowly or nonadaptive receptors.
Pain Transduction by Nociceptors
Noxious stimuli open transduction ion channels in pain receptors which increase membrane permeability to Na+ and/or Ca++ → receptor potential → action potential.
Mechanical stimuli open specific "degenerin" ion channels.
Thermal stimuli open specific "temperature sensing" ion channels.
Chemical stimuli open specific "acid sensing" ion channels.
Pain Sensitizers (OR Chemical mediators of pain)
After the nociceptors are stimulated, the damaged tissues and the surrounding blood vessels release a number of pain and inflammation producing chemical substances that are normally inside the cells, into the ECF.
These substances include: histamine, serotonin, K+, substance P, ATP, bradykinin and prostaglandins.
These substances in particular Prostaglandins- further sensitize the nociceptors, lowering their pain threshold, and producing the primary hyperalgesia that often accompanies pain.
Primary hyperalgesia:
occurs in the injured area and is caused by sensitization of local nociceptors by inflammatory mediators, e.g. in sunburned skin.
Salicylates and other non steroidal anti-inflammatory analgesics (NSAIDs) reduce pain by inhibiting prostaglandin synthesis.
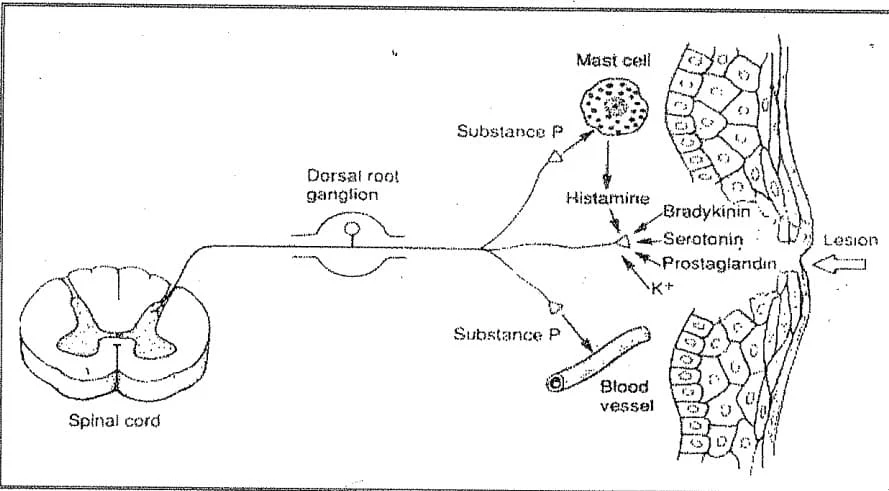 |
| Fig. 1: Chemical mediators of pain |
Threshold of Pain:
Threshold of pain is the same for all people but reaction to pain differs from one person to another
Pain starts to be felt when the skin temperature reaches 45°C, this is considered as average threshold of pain.
Types of Pain sensation:
I- According to site of origin of pain:
- a) Cutaneous pain.
- b) Deep pain.
- c) Visceral pain.
II- According to quality of pain:
Single painful stimuli evoke two successive and qualitatively different sensations referred to as:
a) Fast pain: also called sharp, immediate or first pain. (As fibers)
b) Slow pain: also called dull aching, delayed or second pain.( C fibers)
N.B. The two types of pain can be dissociated from each other by:
- Moderate compression of a nerve trunk will block the Ad fibers leaving the C fibers. The fast pain is lost while the slow type remains.
- Low concentrations of local anaesthetic blocks the C fibers leaving the AS fibers. The slow pain is lost while the fast type remains.
Table 1: Characters and differences between Fast and Slow pain:
| Characteristic | Fast pain | Slow pain |
|---|---|---|
| Type of pain | Sharp, pricking, acute | Dull aching, Burning, throbbing |
| Quality | Immediate | Delayed |
| Onset | Short | Long duration and increase with time |
| Duration | Well localized | Poorly localized (diffuse) |
| Localization | Mechanical & thermal pain receptors | All types of pain receptors |
| Stimulated receptor | Skin and Parietal surfaces | Skin, deep structures and viscera |
| Felt in | Αδ fibers | C fibers |
| Carried by | Hypoxia and compression | Local anaesthesia (e.g. cocaine) |
| Blocked by | Glutamate | Substance P |
| Neurotransmitter | Neo-spinothalamic Tract | Paleo-spinothalamic Tract |
| Pathway | VBN of thalamus | Reticular Formation → intralaminar thalarnic N |
| Relay of 2nd order neurons | PVN of Thalamus | Reticular formation then to Intralaminal Thalamic Nuclues |
| Termination of fibers | Sensory Cortex | The whole Cortex |
| Pain perception | In the Thalamus and Sensory Cortex | Mainly in the Thalamus |
| Motor reflexes | Pressor response | Guarding: hypertonia of overlying muscles |
| Autonomic reactions | Pressor response (Increased heart rate and blood pressure) | Depressor response (Decreased heart rate and blood pressure) |
