Ulcerative colitis is a lifelong inflammatory bowel disease that causes inflammation and ulcers in the colon (large intestine). It is a common type of IBD and differs from Crohn's disease in some of its signs and symptoms.
Ulcerative colitis is characterized by periods of active disease (severe symptoms) and periods of remission (no symptoms).
Differences between ulcerative colitis and Crohn's disease
The external symptoms of the two diseases are similar to a large extent, but clinical examination, X-rays, tests, and endoscopies can clarify the following differences:
- Crohn's disease can affect any part of the digestive tract, starting from the mouth to the anus, while ulcerative colitis affects only the large intestine (colon) and rectum.
- In Crohn's disease, the damaged tissue areas appear as patches of different sizes in the middle of the healthy tissue in the digestive tract, while in ulcerative colitis, the damaged tissue is connected and there are no patches, and it often starts near the anus and extends to the colon.
- Crohn's disease can affect all layers of the affected organ (the inner mucous membrane, the muscle layer, and the outer membrane), while ulcerative colitis affects only the inner mucous membrane layer.
Types of ulcerative colitis
Ulcerative colitis patients can be classified into more than one type as follows:
- Ulcerative proctitis, where the disease includes the last part of the large intestine (rectum)
- Ulcerative proctitis and left-sided colitis (the lower part of the large intestine that resembles the letter "S")
- Left-sided colitis, where the ulcers include the left side of the colon
- Pancolitis, which includes all parts of the colon.
Ulcerative colitis can also be classified according to the severity of the disease, into three degrees: mild, moderate, and severe, taking into account that there is a rare fourth condition called severe ulcerative colitis, which causes severe complications that threaten the patient's life.
Causes of ulcerative colitis
The exact cause of ulcerative colitis is still unknown, but research has shown that it is an autoimmune disease caused by an autoimmune response against the tissues of the digestive tract.
Research has also pointed to the presence of genetic genes in patients with ulcerative colitis, where it is transmitted from parents to children, and some people are genetically predisposed to the disease with a higher percentage than others when they have those genes.
For an unknown reason, when a predisposed person is exposed to certain trigger factors, their immune system begins to attack the cells and tissues of their body instead of attacking the external threat, which causes the destruction of those cells and tissues over the long term.
Risk factors
These are the factors that increase the chances of a person developing ulcerative colitis more than others, and include the following:
- Age: Most patients are diagnosed with this disease in the age group between 15 and 30 years, or those over 60.
- Race and ethnicity: The disease occurs more frequently in people with white skin, especially the Ashkenazi Jewish race.
- Genetic factors: As mentioned above, the risk of someone developing ulcerative colitis increases if one of their first-degree relatives is also affected by the disease.
- Intestinal microbes: These include the bacteria, viruses, and fungi that live in the intestines, the composition of which differs in patients with ulcerative colitis from healthy people. The reasons for the difference are unknown.
Other factors such as stress and diet, do not increase the risk of developing ulcerative colitis, but they cause an increase in the disease's active periods (relapses).
What are the symptoms of ulcerative colitis?
The symptoms of inflammatory bowel disease vary depending on the affected part of the digestive tract, but these symptoms are unfortunately common symptoms with other diseases and are not specific to ulcerative colitis alone, so they are not relied upon alone in diagnosis.
Those symptoms include the following:
- Abdominal pain: due to abdominal cramps or what is called "cramps".
- Irregular bowel movements, alternating between constipation and diarrhea, with the passage of mucus with stool without blood
- Continuous weight loss
- Episodes of fever (high temperature) and sweating
- General fatigue and a constant feeling of fatigue and the desire to rest or sleep
- Occasional joint pain
- In children: If the disease starts in childhood, it causes delayed growth and can also cause incomplete sexual development
- Extraintestinal symptoms: occur in 10-20% and include symptoms of iritis and liver infections
- Bloody stool: means the appearance of blood in the stool, and is usually accompanied by "tenesmus" (the urge to defecate without stool), and occurs more frequently with ulcerative colitis and less frequently with Crohn's disease
The World Gastroenterology Organization (WGO) considered the following symptoms to be a sign of tissue damage in the digestive tract:
- Diarrhea: with mucus or blood in the stool, and it often occurs at night and may be accompanied by weakness in the control of the anal sphincter.
- Constipation: Constipation may be the first symptom of ulcerative colitis if it occurs in the rectum, and it may extend to the extent of intestinal obstruction.
- Bowel movement disorders: May occur disorders such as tenesmus and frank bleeding from the rectum with pain in the lower abdomen and a strong urge to defecate.
- Vomiting and nausea: They occur more frequently in cases of Crohn's disease than ulcerative colitis.
How is ulcerative colitis diagnosed?
In addition to the medical history and the symptoms mentioned above, when the doctor examines the patient clinically, he finds the following medical signs:
- Fever (high temperature)
- Increased heart rate
- Signs of dehydration and signs of poisoning
- Pale skin and some signs of anemia (anemia)
- Toxic megacolon: It is considered a medical emergency where pus occurs in the blood and the patient suffers from severe fever, chills, severe lethargy with increased heart rate, ascending pain in the abdomen with severe bloating.
Tests required for diagnosis
Despite the existence of a large number of tests that can help diagnose inflammatory bowel disease, unfortunately there is no specific analysis that can confirm the diagnosis, so colonoscopy is resorted to in most cases. The following tests can be performed to reach the correct diagnosis, in addition to evaluating the impact of the disease on the general condition of the patient, and the doctor chooses from them what suits the case:
- Complete blood count
- Fecal calprotectin analysis
- Nutritional assessment tests: measuring vitamin B12 levels, and measuring iron levels in the blood with determining folic acid levels.
- Analysis of erythrocyte sedimentation rate and C-reactive protein (CRP)
- ANCA and ASCA analysis
- Stool culture and tests for worm examination
Radiology:
- Barium enema via rectal injection
- Computed tomography scan of the abdomen and pelvis
More advanced tests:
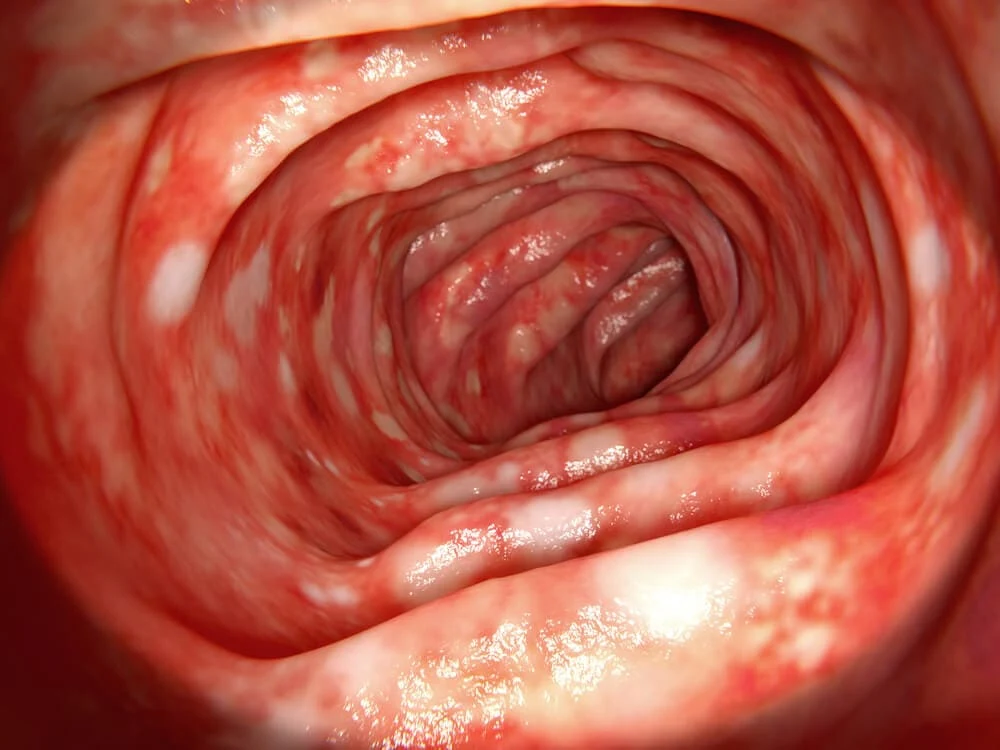
- Colonoscopy with tissue sampling
- Flexible colonoscopy
- Upper endoscopy, stomach and small intestine endoscopy (in case of suspicion of Crohn's disease)
- Double-balloon endoscopy of the digestive tract
Treatment approach
The internationally approved treatment plan depends on the stage the disease has reached, and there are also differences in treatment between Crohn's disease and ulcerative colitis, as will be detailed. The treatment plan begins by treating the symptoms to relieve pain, eliminate vomiting, diarrhea, and bowel disorders, while treating the internal effects of the disease in mild cases, and then the treatment plan is developed and escalated step by step until the desired response is achieved.
The following are options for treating inflammatory bowel disease:
Line 1: Aminosalicylates (Aminosalicylates): These medications are taken orally, as a rectal suppository, or with an enema. They are the basis of treatment for periods of remission and activity of the disease and aim to keep the disease in a state of remission. These medications are more suitable for the treatment of ulcerative colitis.
Line 1a: Antibiotics are used in limited cases of ulcerative colitis to avoid increasing inflammation (the Pseudomonas bacteria is activated due to the use of antibiotics in the colon).
Line 2: Corticosteroids are used only in cases of relapse (activity of the disease).
Line 3: Immunomodulators and biologics are considered the last drug line for patients who do not respond to the previous two lines or have contraindications to their use.
Surgery
Surgery can be used in cases of ulcerative colitis by resecting the affected parts of the colon and reconnecting it. Surgery may reach the extent of resection of the entire colon and rectum and making a special bag to defecate through it. Surgery is not a therapeutic solution in cases of Crohn's disease, but it may be resorted to in some cases only to prevent complications such as narrowing of the digestive tract or the possibility of obstruction.
What are the potential complications of inflammatory bowel disease?
There are some potential complications that may occur for patients with inflammatory bowel disease, they are not guaranteed to occur but they can appear in varying proportions, especially in cases that neglect treatment, those complications are:
- Cancer: Patients with inflammatory bowel disease are more at risk of developing colon cancer than others.
- Anal fistula: A tunnel that arises under the skin and connects the rectum to the anus.
- Stricture of the rectum and anus, which may lead to difficulty and pain when defecating.
- Anemia: as a result of continuous blood loss through bleeding inside the digestive tract.
- Kidney stones
- Liver cirrhosis and inflammation of the bile ducts
- Symptoms of malnutrition due to poor absorption of food due to damage to intestinal tissue
- Osteoporosis
- Intestinal perforation
- Toxic megacolon