Definition: Simply it is bleeding from the nose. or acute haemorrhage from nasal cavity, nostrils or even the nasopharynx.
Etiology:
a. Local causes:
1. Idiopathic:
- Commonest cause (90%).
- May be precipitated by minor trauma or hot atmosphere.
- Bleeding from little’s area (Kiesselbach’s plexus), which is the anterior part of the septum where septal branch of sphenopalatine, anterior ethmoidal, greater palatine & superior labial branch of facial artery anastomose, most site exposed to cold dry air and crustations.
2. Traumatic:
- Foreign body, fracture nose, and fracture skull base.
- Iatrogenic; Functional endoscopic sinus surgery, Septoplasty, Turbinate resection, Nasotracheal intubation and Nasogastric tube.
3. Inflammatory:
- All cases of acute, and chronic rhinitis, and sinusitis may be associated with varying degree of epistaxis.
- Nasal granulomas.
4. Neoplastic:
a) Tumors of the nose & sinuses:
- Benign: hemangioma - Malignant
b) Tumors of the nasopharynx:
- Benign: angiofibroma - Malignant: carcinoma & sarcoma.
5- Deviated septum:
- Convex side angulated vessels
- Concave side mucosal dryness
- Septal perforation
6- Hereditary hemorrhagic telangiectasia.
b. General Causes:
1. Cardio-vascular causes:
- High arterial pressure (hypertension): Commonest cause in elderly, usually it is posterior bleeding. Hypertension does not initiate but maintain bleeding.
- High venous pressure: Heart failure, mitral stenosis, emphysema, or mediastinal masses.
2. Blood diseases:
Purpura, hemophilia, leukemia, thrombocytopenia.
3. Drugs:
- Anticoagulants, e.g. heparin.
- Antiplatelet e.g. aspirin, NSAID.
4. Hepatic
Liver failure >> hypoprothrombinemia.
5. Fever
E.g. Exanthemata: rheumatic fever & infective endocarditis >> vasculitis.
Management of Epistaxis :
I- First Aid:
- Patient is managed in seated position with head slightly flexed and leaning forward unless shocked (supine with head down).
- Pinch the nose between index & thumb.
- Apply cold compresses to the forehead.
- Patient is asked to spit blood not to swallow it.
- Insert a piece of cotton soaked with a vasoconstrictor solution (Epinephrine 1/100, 1000) into nostrils for 5-10m. (avoided in hypertensive & cardiac patients).
II- Assessment:
a. History of the cause
b. Examination for:
1. Site: Unilateral or bilateral, Anterior or posterior.
Sites:
- Little‘s area (90%).
- Upper part above middle turbinate: (anterior, posterior ethmoidal >> (ICA).
- Posterior part below middle turbinate: (Sphenopalatine >> ECA).
NB. Rigid endoscope may be used.
2. Severity.
3. Shock: Weak rapid pulse, hypotension, tachypnea, pallor, cold, sweating, Irritability, and low urine output.
4. Cause.
III- Control bleeding:
(A) Mild bleeding:
1. General first aid.
2. Cauterization:
- When bleeding stops or diminishes.
- Under: local A. 4% cocaine or xylocaine.
- By: Electrical: more effective, Chemical: silver nitrates or chromic acid.
- Then: avoid manipulation, lubricant nasal drops for 1 week.
3. Nasal packing if bleeding continues after cautery.
(B) Severe bleeding:
Stop bleeding by packing + control shock
1. Anterior nasal packing:
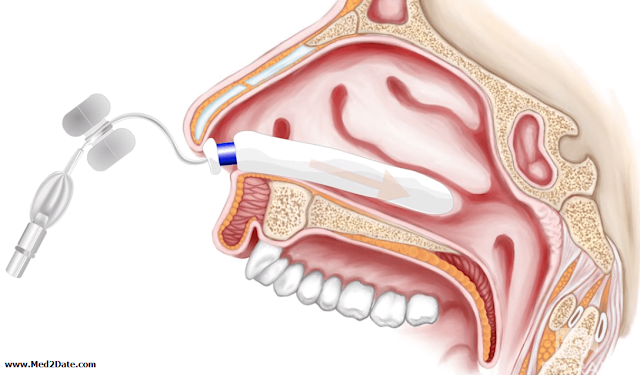
- Nasal packing can be used to control active bleeding as a tamponade using absorbable (as gelatin, carboxymethyl-cellulose, oxidized cellulose, hyaluronic acid, fibrillar collage) and nonabsorbable packs (as ribbon gauze, folly’s catheter, inflatable rubber tampon, or Mirocell) according to availability and clinician preference.
- Original packing was a strip of ribbon gauze 50 X 2.5cm, impregnated with Vaseline, lignocaine & antibiotic ointment, apply surface anesthesia, introduced in layers.
2. Posterior nasal packing:
- If anterior packing fails to control bleeding.
- Under general anasthesia.
- Piece of gauze with antiseptic ointment lodged firmly in the nasopharynx with 2 threads coming from the nostrils & tied together and a third one coming from the mouth
- Left for 24-48h.
- Give antibiotics.
- Alternatively: Foley’s catheter.
3. General measures:
- Coagulants e.g. vitamin k, fresh plasma.
- Antibiotics.
- Sedation e.g. diazepam -Transfusion blood, fluids.
- Rest in bed supine position.
- Observation of vital signs, Hemoglobin %, blood gases &urine.
4. Arterial ligation:
If all previous measures failed, or recurrent epistaxis despite repeated packing.
- Ethmoidal artery ligation via external frontoethmoidectomy approach or endoscopically (if bleeding coming from above middle turbinate).
- Sphenopalatine artery ligation or cautery using endoscope.
- Maxillary artery ligation Via transantral approach (if bleeding coming from below middle turbinate): more effective than ECA ligation.
- ECA ligation.
5. Arterial embolization:
During angiography by gelfoam, polyvinyl alcohol or coiling.
IV- Management of the cause:
(A) Investigations:
- Coagulation profile B.T, C.T, PT, PC, PTT.
- Blood picture.
- C.T & biopsy from a nasal mass.
(B) Treatment of the cause:
- Bleeding from the little's area: it is usually controlled by cauterization either chemically using silver nitrates or electrocautery (N.B. don't cauterize two opposite sides of the septum to avoid septal perforation)
- Hypertension: use antihypertensive drugs.
- Tumors especially angiofibroma: endoscopic excision.
- Deviated septum or septal perforation: septal surgery.
- Hereditary hemorrhagic telangiectasia: laser photocoagulation, bipolar cauterization, systemic hormone therapy, or septodermoplasty.
- Defect in coagulation: treat the cause.