Treatment strategies of respiratory syncytial virus infection are largely supportive, with a focus on ensuring adequate oxygenation, ventilation, nutrition, and hydration.
No available treatment shortens the course of bronchiolitis or hastens the resolution of symptoms.
High-risk infants include those with a history of prematurity, age <6 months at the start of RSV season, chronic lung disease, complex congenital heart disease, or immune deficit.
These patients require closer observation and are frequently admitted to hospital.
Treatment strategies depend on the severity of the illness.
For adults, management is typically limited to supportive care, with supplemental oxygen, bronchodilators, intravenous fluids, and antipyretics as required and guided by the individual clinical scenario.
Antiviral therapy may be considered for patients following solid organ or haematopoietic stem cell transplantation to prevent progression to lower respiratory tract involvement.
Hospitalisation and supportive care
Mild illness
- Patients have no hypoxaemia and can feed adequately.
- For most infants, RSV disease is usually mild and self-limiting and can be treated in the outpatient setting. Outpatient care requires diligent follow-up to ensure that the patient is not deteriorating.
- High-risk infants (e.g., history of prematurity, age <6 months at start of RSV season, chronic lung disease, complex congenital heart disease, or immune deficit) may require hospital admission.
- Treatment is largely supportive and about providing adequate nutritional support. Infants are obligate nose breathers, and nasal obstruction is a frequent problem. Simple nasal toilet with saline drops and a suction bulb can significantly improve the work of breathing.
- Symptomatic therapy for healthy adults is usually sufficient, as the disease is typically confined to the upper respiratory tract and is self-limiting.
- Signs of moderate illness in infants include hypoxaemia (oxygen saturations <90-92%), tachypnoea, increased work of breathing (nasal flaring, intercostal retractions, head bobbing), inadequate feeding, and dehydration.
- Patients should be admitted for further care and observation.
- Hypoxaemia should be treated with warm, humidified oxygen through a nasal cannula or mask.
- High-flow nasal cannula (HFNC) therapy is safe in a typical ward setting. However, there is no clear evidence that initiating support with HFNC is more effective than standard oxygen therapy with a mask, either in shortening hospital length-of-stay or preventing ICU admissions (although studies have been conflicting). HFNC should be limited to infants who have failed standard oxygen therapy.
- Careful attention should be given to prompt correction of any dehydration and re-establishing adequate nutrition. Infants with poor feeding or significantly elevated work of breathing or respiratory rate should be fed by nasogastric or nasojejunal tube, or receive intravenous fluids.
- Adults who are older, immune deficient, or have comorbidities may have moderate illness and should be managed with supportive care while addressing exacerbations of underlying illnesses.
Severe illness
- Infants with refractory hypoxaemia, progressive respiratory distress, or frank respiratory failure should be transferred to the paediatric intensive care unit.
- These patients often improve with non-invasive mechanical ventilation such as nasal continuous positive airway pressure or non-invasive ventilation, but may require endotracheal intubation with mechanical ventilation. These modalities are associated with significantly decreased RSV-associated mortality.
- Hypoxaemia should be treated with warm, humidified oxygen through a nasal cannula or mask.
- Rehydration and nutrition can be accomplished by enteral or parenteral routes, depending on the degree of disease severity and other clinical considerations. In the UK, the National Institute for Health and Care Excellence recommends giving fluids by nasogastric or orogastric tube in babies and children with bronchiolitis if they cannot take enough fluid by mouth. Alternatively, it recommends intravenous isotonic fluids to babies and children who do not tolerate nasogastric or orogastric fluids or have impending respiratory failure.
- Adults who are older, immune deficient, or have comorbidities may progress to severe illness, requiring intensive care unit admission with respiratory support and intravenous and nutritional support.
↚
Adjunctive therapies
Bronchodilators
- Bronchodilators (e.g., salbutamol and ipratropium) should not be used routinely in the management of bronchiolitis.
- Bronchodilators may be of benefit for patients with asthma, COPD, or severe disease.
- Bronchodilators may transiently improve oxygen saturation and work of breathing, but have not been shown to decrease hospital admissions, length of stay, or length of oxygen therapy.
- Nebulised hypertonic saline is of potential benefit in reducing symptoms of mild or moderate bronchiolitis in the hospital setting.
- Given the relatively long period of use required to achieve improvement, nebulised hypertonic saline is not recommended for use in the accident and emergency department.
Ribavirin ± intravenous immunoglobulin (IVIG)
- Ribavirin is not recommended for routine use in children with bronchiolitis.
- Ribavirin is a synthetic nucleoside analogue with in vitro activity against RSV. In practice, however, its benefit is less certain.
- Several factors complicate the use of ribavirin: it is expensive; it must be given early in the course of infection for best effect; it may present a risk to those who give it, as it is a potential teratogen when administered by nebulisation.
- Oral ribavirin has been used in immune deficient adults (predominantly transplant recipients and cancer patients with severe RSV disease), although it is not approved for this indication. Its early use in adult bone marrow transplant patients has reduced morbidity and mortality in this patient subset.
- IVIG may be added to inhaled ribavirin for immune deficient patients at high risk for progression to severe lower respiratory tract disease. IVIG with oral ribavirin has also been studied in immune deficient patients.
- One review reported that recipients of dual therapy (aerosolised ribavirin with either IVIG or palivizumab) had less progression to lower respiratory tract infection than those patients who received aerosolised ribavirin alone. Use of IVIG or RSV-immunoglobulin treatment alone did not significantly shorten the duration of hospitalisation of infants with RSV bronchiolitis and/or pneumonia.
- Studies with aerosolised ribavirin therapy demonstrated a small increase in oxygen saturation in small clinical trials; however, a decrease in the need for mechanical ventilation or a decrease in the length of stay was not shown. Because of limited evidence for a clinically relevant benefit, potential toxic effects, and high cost, routine use of aerosolised ribavirin is not recommended.
Antibiotics
- Routine administration of empirical antibiotic therapy to infants with RSV bronchiolitis is not recommended, because the risk of concomitant bacterial infection is very low (0.2%).
- Antibiotics should be administered to those with confirmed or strongly suspected bacterial infections.
- For infants with severe RSV bronchiolitis who require intubation, the risk of bacterial pneumonia is significantly higher (26%). These infants may benefit from initiation of antibiotics pending culture results.
Corticosteroids
- Corticosteroids are not effective in the routine management of RSV infection and do not appear to reduce subsequent recurrent wheeze or asthma. In addition, their use in patients with bronchiolitis indicate that they do not reduce hospital admissions and do not reduce length of stay for inpatients.
- The American Academy of Pediatrics guidelines and the Scottish Intercollegiate Guidelines Network guidelines on the management of bronchiolitis recommend against the routine use of corticosteroids for this condition.
- Corticosteroids may be beneficial in patients with atopy, asthma, or chronic lung disease.
Less effective or ineffective therapies
- Chest physiotherapy has not been shown to improve outcomes, and its use is discouraged. In the UK, the National Institute for Health and Care Excellence does not recommend chest physiotherapy on babies and children with bronchiolitis. However, a chest physiotherapy assessment in babies and children who have relevant comorbidities where there may be additional difficulty clearing secretions (e.g., spinal muscular atrophy, severe tracheomalacia) may be warranted.
- Mucolytic therapy with nebulised recombinant human DNase, acetylcysteine, or carbocisteine has not been effective.
- Surfactant therapy for intubated patients has not been effective.
- Helium-oxygen (heliox) mixtures have shown no benefit in regards to the rate of intubation, rate of accident and emergency department discharge, or length of treatment for respiratory distress in the management of bronchiolitis in infants.
- Montelukast has not been proven effective in the treatment of RSV infection, or in the reduction of post-bronchiolitis wheezing.
- Evidence is lacking for the safety and effectiveness of magnesium sulphate in children ≤2 years with bronchiolitis.
Treatment algorithm
Treatment is recommended as follows:
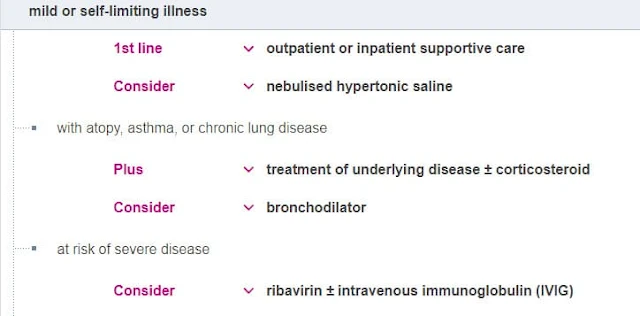
a. Self-limiting (Mild) ilness:
For most infants RSV disease is usually mild and self-limiting, and can be treated in the outpatient setting. Outpatient care requires diligent follow-up to ensure that the patient is not deteriorating.Treatment is largely supportive regardless of setting, with a focus on improving oxygenation and ventilation and providing adequate nutritional support. No available treatment shortens the course of bronchiolitis or hastens the resolution of symptoms.
Infants are obligate nose breathers, and nasal obstruction is a frequent problem. Simple nasal toilet with saline drops and a suction bulb can significantly improve the work of breathing.
High-risk infants include those with history of prematurity, age under 6 months at start of RSV season, chronic lung disease, complex congenital heart disease, or immune deficit. These patients require closer observation and, frequently, admission to hospital.
Symptomatic therapy for healthy adults is usually sufficient, as the disease is usually confined to the upper respiratory tract and is self-limiting.
For adults with mild RSV illness, therapy is also largely supportive and targeted at relieving symptoms.
Nebulised hypertonic saline is of potential benefit in reducing symptoms of mild or moderate bronchiolitis in the hospital setting.
Given the relatively long period of use required to achieve improvement, nebulised hypertonic saline is not recommended for use in the accident and emergency department
b. Moderate ilness:
Hypoxaemia should be treated with warm, humidified oxygen through nasal cannula or mask.
High-flow nasal cannula (HFNC) support is safe in a typical ward setting. There is no clear evidence that initiating support with HFNC is more effective than standard oxygen therapy with a mask, either in shortening hospital length-of-stay or preventing ICU admissions, although studies have been conflicting.
Given the current state of uncertainty and the higher resources needed for HFNC therapy, its use outside of clinical trials should be limited to infants who have failed standard oxygen therapy.
Careful attention should be given to intravascular fluid and nutritional support. Infants with poor feeding or significantly elevated work of breathing or respiratory rate should be fed by nasogastric or nasojejunal tube or receive intravenous fluids.
High-risk infants include those with a history of prematurity, age under 6 months at start of RSV season, chronic lung disease, complex congenital heart disease, or immune deficit. These patients require closer observation and, frequent admission to hospital.
Adults who are older, immune deficient, or have comorbidities may have moderate illness and should be managed with supportive care while exacerbations of underlying illnesses are addressed.
c. Severe ilness:
Emerging treatments
Vaccines
No vaccine has been licensed to prevent RSV infection.
Difficulties encountered in RSV vaccine development include: ineffective protective immunity arising from natural infection; difficulty establishing end point metrics for measuring vaccine response; the need for rigorous safety analysis due to enhanced disease severity associated with the formalin-inactivated RSV vaccine.
However, several promising vaccines targeting infants, older people, and pregnant mothers are in clinical development and several reports provide a comprehensive summary of various vaccine candidates.
Most target the fusion glycoprotein (F) of RSV. Of these, an insect cell-derived RSV F nanoparticle vaccine candidate shows the most potential.
A phase 3 clinical trial for use in pregnant women with the expectation of conferred immunity to the fetus failed to achieve the primary outcome measure, but showed some promise in reducing RSV associated disease in the babies.
The Food and Drug Administration (FDA) has granted fast-track designation to the RSV F nanoparticle vaccine (for the protection of infants and adults >60 years) and breakthrough designation to an adenovirus serotype 26 (Ad26)-based respiratory syncytial virus (for patients aged 65 years and older).
Other vaccines including adjuvanted respiratory syncytial virus F protein are at earlier stages of clinical development.
To date, RSV vaccines are well tolerated and no significant adverse events have been reported.
However, several have failed to meet primary end points of preventing clinical disease.
Nirsevimab
Nirsevimab, an investigational monoclonal antibody that targets the RSV fusion protein has been granted PRIME (PRIority MEdicines scheme) designation by the European Medicines Agency and breakthrough therapy designation by the FDA for the prevention of lower respiratory tract infections caused by RSV infections in infants. Nirsevimab has an extended half-life (117 days), and is intended to protect infants for an entire RSV season with a single intramuscular dose.
In healthy preterm infants, nirsevimab resulted in fewer hospitalisations for RSV-associated lower respiratory tract infections compared with placebo.
A phase 3 trial found that a single dose of nirsevimab provided protection against medically attended RSV-associated lower respiratory tract infection when given to healthy late-preterm and term infants before an RSV season. Nirsevimab is not commercially available as yet.
Novel antiviral compounds
Several antiviral compounds are in clinical development. These include therapies blocking RSV fusion protein (RSV-F) , inhibiting viral polymerase (RSV-L), or other central viral proteins (RSV-N , RSV-M2).
These therapies are at various stages of clinical development. Sisunatovir, an orally available inhibitor of the RSV fusion (RSV-F) protein, has been granted fast track designation by the US Food and Drug Administration.